Being “too much” is what finally led me to health—and—and it’s backed by science.
Chronically Holistic

For years, I lived by elimination—cutting out foods, habits, and even parts of myself. But healing didn’t truly begin until I shifted to addition—intentionally nurturing what my nervous system needed: safety, faith, nourishment, and calm.
Scientific research now confirms what holistic practitioners have long observed: early-life stressors—from complex births and environmental toxins to prolonged insecurity—can deeply impact long-term health. A landmark review shows that those exposed to major psychological stressors in early life face elevated rates of chronic diseases and diminished longevity PMC. Another investigation specifically links childhood adversity with increased risk of chronic illnesses across adulthood ScienceDirect+1.
Even on a neurobiological level, early-life stress alters brain development, particularly in circuits that govern stress response, emotion regulation, and memory. These changes in the prefrontal cortex, amygdala, hippocampus—and in stress-hormone pathways—can lead to heightened vulnerability across life BioMed Central.
I’ve been a nurse for 9 years, working primarily in emergency medicine with a focus on pediatrics. I entered this demanding field while still recovering—on multiple prescriptions, frequenting specialists, and healing from surgeries. Every day, I witnessed people in crisis, and I often minimized my own suffering in comparison.
But what goes on outside the hospital doors—in our homes—might matter even more. Health is built every day, not just in moments of extreme illness. Diet, stress coping, environmental quality, and resources are foundational—but often undervalued elements.
Consider sleep health, for instance. Environmental factors—like air pollution, noise, ambient light, and neighborhood safety—play a significant role in shaping sleep patterns and disorders, especially in socioeconomically disadvantaged communities PMCAJMC.
On a broader scale, the social determinants of health—poverty, education, employment, and living conditions—have a more substantial impact on outcomes than clinical care alone ASPE.
Even nutrition doesn’t operate in a vacuum. A recent study examining reproductive-age adults revealed that lifestyle patterns (diet quality, scheduling, eating behaviors) are strongly tied to social factors like rural vs. urban living, employment status, and daily routines MDPI.
Why This Matters
- Early trauma isn’t just emotional—it’s biological, reshaping your brain, hormones, and immune system in ways that last a lifetime.
- True health isn’t born in ER rooms—it’s nurtured daily through safety, rest, nutrition, clean environments, and meaningful connection.
- You aren’t inherently broken and don’t need to be medication-deficient—you deserve access to basic human rights: nourishing food, fresh air, trust, and community.
Next Steps: Nourishing the Nervous System
Healing isn’t just about avoiding harm—it’s about providing the body with what it truly needs. The Emotion Code reminds us that trapped emotions and unprocessed stressors can keep the nervous system locked in “fight or flight.” Pairing emotional release techniques with nutritional support builds resilience at the cellular and emotional level.
Foundational Nutritional Support
- Magnesium-rich foods (leafy greens, pumpkin seeds, avocado) — critical for calming the nervous system, relaxing muscles, and reducing anxiety.
- Omega-3 fatty acids (wild salmon, sardines, flaxseed, walnuts) — shown to support mood regulation, reduce inflammation, and stabilize neuronal membranes.
- B vitamins (grass-fed liver, eggs, beef, dark leafy greens) — essential for neurotransmitter synthesis and energy production.
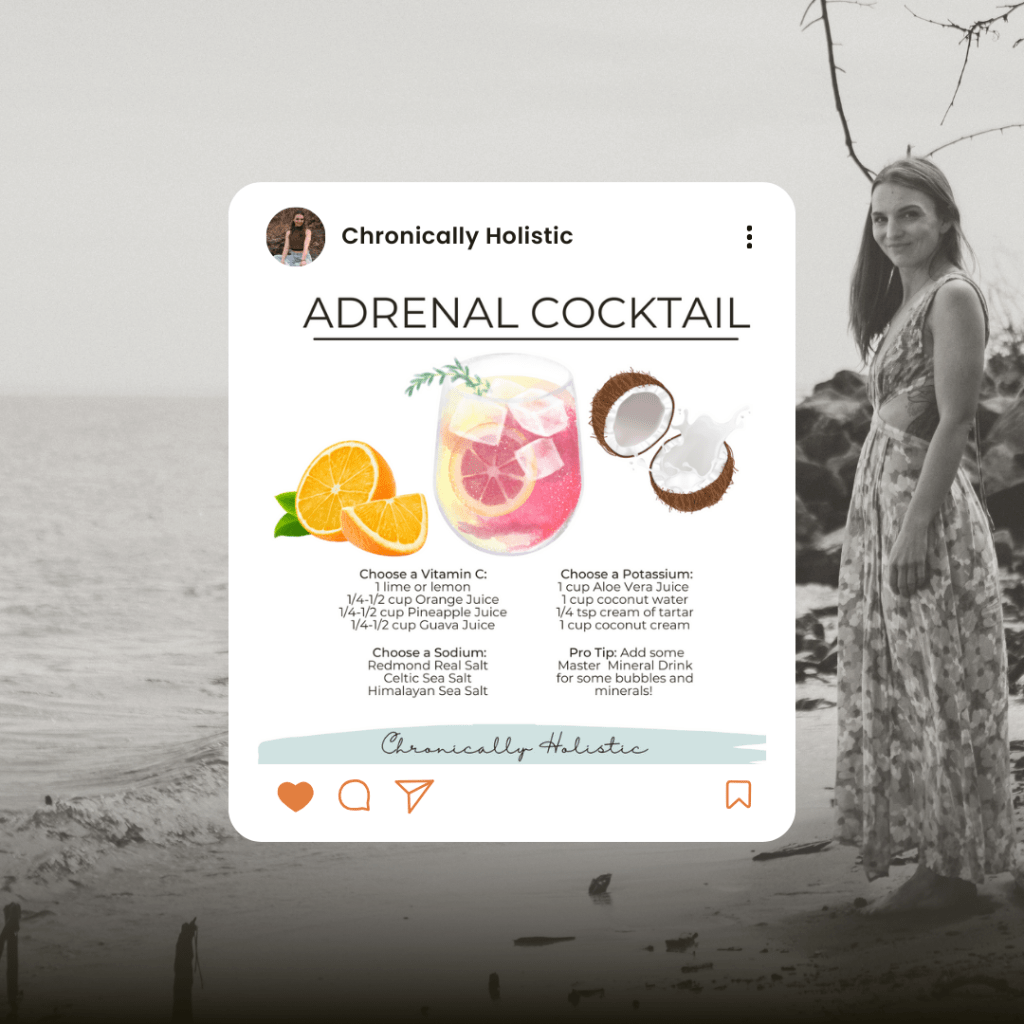
- Mineral-dense foods (bone broth, sea salt, kelp, beets) — restore electrolytes, supporting adrenal function and overall resilience.
- Whole-food vitamin C sources (citrus, kiwi, bell peppers, acerola cherry) — vital for adrenal repair and nervous system balance

Nervous System Practices
- Heart-focused breathing — slowing and deepening the breath signals safety to the vagus nerve.
- Grounding foods + grounding habits — root vegetables and mindful movement help the body feel safe and supported.
- Releasing trapped emotions (The Emotion Code technique) — identifying and processing unresolved emotional energies allows the body to shift out of chronic stress.
- Daily safety rituals — creating a calm environment, practicing gratitude, and limiting toxic inputs (chemicals, negative media, processed food) reinforces stability.
The Takeaway
Your nervous system doesn’t need more stimulation—it needs restoration. True resilience is built when emotional release, nutrient density, and nervous system support come together.
✨ Ready to uncover what your body truly needs? Let’s work 1:1 to identify your deficiencies and support your nervous system. Connect with me here: chronicallyholistic.com/how-to-work-with-me
Book a free 15 minute consultation here: Schedule Your Call